Disease progression
Abscesses can recur if the fistula seals over, allowing the accumulation of
pus. It can then extend to the surface again repeating the process. Anal
fistulae per se do not generally harm, but can be very painful, and can be
irritating because of the drainage of pus (it is also possible for formed stools
to be passed through the fistula). Additionally, recurrent abscesses may lead to
significant short term morbidity from pain and, importantly, create a starting
point for systemic infection.
Treatment, in the form of surgery, is considered essential to allow drainage and prevent infection. Repair of the fistula itself is considered an elective procedure which many patients opt for due to the discomfort and inconvenience associated with an actively draining fistula.
Signs and symptoms
- skin maceration
- pus, serous fluid and/or (rarely) feces discharge can be bloody or
purulent
- pruritus ani itching
- depending on presence and severity of infection:
- - pain
- - swelling
- - tenderness
- - fever
- - unpleasant odor
- Thick discharge, which keeps the area wet
Diagnosis
Diagnosis is by examination, either in an outpatient setting or under anaesthesia (referred to as EUA or Examination Under Anaesthesia). The fistula may be explored by using a fistula probe (a narrow instrument). In this way, it may be possible to find both openings. The examination can be an anoscopy. Diagnosis may be aided by performing a fistulogram, proctoscopy and/or sigmoidoscopy.
Possible findings:
- The opening of the fistula onto the skin may be observed
- The area may be painful on examination
- There may be redness
- An area of induration may be felt; thickening due to chronic infection
- A discharge may be seen
Classification of types of anal fistula
Depending on their relationship with the internal and external sphincter muscles, fistulae are classified into five types:
Extrasphincteric fistulae begin at the rectum or sigmoid colon and proceed downward, through the levator ani muscle and open into the skin surrounding the anus. Note that this type does not arise from the dentate line (where the anal glands are located). Causes of this type could be from a rectal, pelvic or supralevator origin, usually secondary to Crohn's disease or an inflammatory process such as appendiceal or diverticular abscesses.
Suprasphincteric fistulae begin between the internal and external sphincter muscles, extend above and cross the puborectalis muscle, proceed downward between the puborectalis and levator ani
muscles, and open an inch or more away from the anus.
Transphincteric fistulae begin between the internal and external sphincter muscles or behind the anus, cross the external sphincter muscle and open an inch or more away from the anus.
These may take a 'U' shape and form multiple external openings. This is
sometimes termed a 'horseshoe fistula'.
Intersphincteric fistulae begin between the internal and external sphincter
muscles, pass through the internal sphincter muscle, and open very close to the
anus.
Submucosal fistulae pass superficially beneath the submucosa and do not cross either sphincter muscle.
Treatment
There are several stages to treating an anal fistula:
Definitive treatment of A fistula aims to stop it recurring. Treatment depends on where the fistula lies, and which parts of the internal and external anal sphincters it crosses.
Lay-open of fistula-in-ano this option involves an operation to cut the fistula open. Once the fistula has been laid open it will be packed on a daily basis for a short period of time to ensure that the wound heals from the inside out. This option leaves behind a scar, and depending on the position of the fistula in relation to the sphincter muscle, can cause problems with incontinence. This option is not suitable for fistulae that cross the entire internal and external anal sphincter.
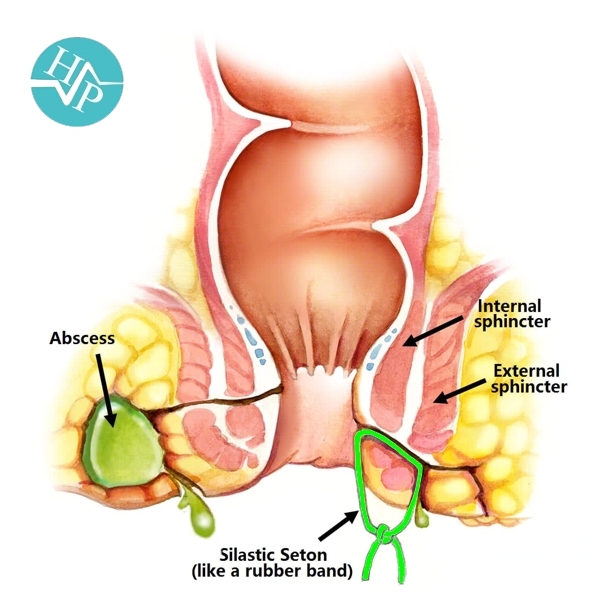
Cutting seton if the fistula is in a high position and it passes through a significant portion of the sphincter muscle, a cutting seton (from the Latin seta, "bristle") may be used. This involves inserting a thin tube through the fistula tract and tying the ends together outside of the body. The seton is tightened over time, gradually cutting through the sphincter muscle and healing as it goes. This option minimizes scarring but can cause incontinence in a small number of cases, mainly of flatus. Once the fistula tract is in a low enough position it may be laid open to speed up the process, or the seton
can remain in place until the fistula is completely cured. This was the
traditional modality used by physicians in Ancient Egypt and formally codified
by Hippocrates, who used horsehair and linen.
Seton stitch a length of suture material looped through the fistula which keeps it open and allows pus to drain out. In this situation, the seton is referred to as a draining seton. The stitch is placed close to the ano-rectal ring which encourages healing and makes further surgery easy.
Fistulotomy The most common type of surgery for anal fistulas is a fistulotomy. This involves cutting along the whole length of the fistula till anorectal ring to open it up so it heals as a flat scar.
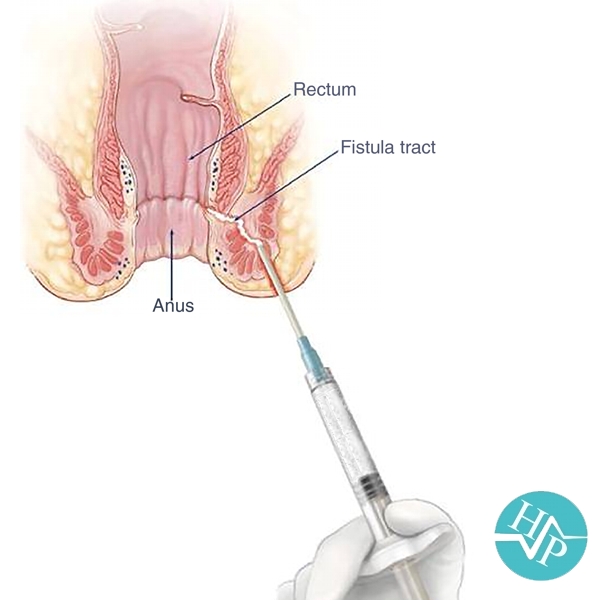
Fibrin glue injection is a method explored in recent years, with variable success. It involves injecting the fistula with a biodegradable glue which should, in theory, close the fistula from the inside out, and let it heal naturally. This method is perhaps best tried before all others since, if successful, it avoids the risk of incontinence, and creates minimal stress for the patient.
Fistula plug involves plugging the fistula with a device made from small intestinal submucosa. The fistula plug is positioned from the inside of the anus with suture. According to some sources, the success rate with this method is as high as 80%. As opposed to the staged operations, which may require multiple hospitalizations, the fistula plug procedure requires hospitalization for only about 24 hours. Currently, there are two different anal fistula plugs cleared by the FDA for treating ano-rectal fistulae in the United States. This treatment option does not carry any risk of bowel incontinence. In the systematic review published by Dr Pankaj Garg,
the success rate of the fistula plug is 65-75%.
Endorectal advancement flap is a procedure in which the internal opening of the fistula is identified and a flap of mucosal tissue is cut around the opening. The flap is lifted to expose the fistula, which is then cleaned and the internal opening is sewn shut. After cutting the end of the flap on which the internal opening was, the flap is pulled down over the sewn internal opening and sutured in place. The external opening is cleaned and sutured. Success rates are variable and high recurrence rates are directly related to previous attempts to correct the fistula.
LIFT Technique is a novel modified approach through the intersphincteric plane for the treatment of fistula-in-ano, known as LIFT (ligation of intersphincteric fistula tract) procedure. LIFT procedure is based on secure closure of the internal opening and removal of infected cryptoglandular tissue through the intersphincteric approach. Essential steps of the procedure include, incision at the intersphincteric groove, identification of the intersphincteric tract, ligation of intersphincteric tract close to the internal opening and removal of intersphincteric
tract, scraping out all granulation tissue in the rest of the fistulous tract,
and suturing of the defect at the external sphincter muscle. The procedure was developed by Thai colorectal surgeon, Arun Rojanasakul,
The first reports of preliminary healing result from the procedure were 94% in
2007. Additional ligation of the intersphincteric fistula tract did not improve the outcome after endorectal
advancement flap.
Fistula clip closure (OTSC Proctology) is a recent surgical development, which involves the closure of the internal fistula opening with a superelastic clip made of nitinol (OTSC). During surgery, the fistula tract is debrided with a special fistula brush and the clip is transanally applied with the aid of a preloaded clip applicator. The surgical principle of this technique relies on the dynamic compression and permanent closure of the internal fistula opening by the superelastic clip. Consequently, the fistula tract dries out and heals instead of being kept open by continuous feeding with stool and fecal organisms. This minimally-invasive sphincter-preserving technique has been developed and clinically implemented by the German surgeon Ruediger Prosst.
First clinical data of the clip closure technique demonstrate a success rate of
90% for previously untreated fistulae and a success rate of 70% for recurrent
fistulae.
Video-assisted anal fistula treatment (VAAFT) is a surgical kit for treating anal fistulae. The system comprises:
- - A video telescope (fistuloscope) to allow surgeons to see inside the fistula tract.
- - A unipolar electrode for diathermy of the internal tract. This is connected to a high frequency generator.
- - A fistula brush and forceps for cleaning the tract and clearing any granulation tissue.
The VAAFT procedure is done in 2 phases, diagnostic and operative. Before the procedure, the patient is given a spinal or general anaesthetic and is placed in the lithotomy position (legs in stirrups with the perineum at the edge of the table). In the diagnostic phase, the fistuloscope is inserted into the fistula to locate the internal opening in the anus and to identify any secondary tracts or abscess cavities. The anal canal is held open using a speculum and irrigation solution is used to give a clear view of the fistula tract. Light from the fistuloscope can be seen from inside the anal canal at the location of the internal opening of the fistula, which helps to locate the internal opening. In the operative phase of the procedure, the fistula tract is cleaned and the internal opening of the fistula is sealed. To do this, the surgeon uses the unipolar electrode, under video guidance, to cauterise material in the fistula tract. Necrotic material is removed at the same time using the fistula brush and forceps, as well as by continuous irrigation. The surgeon then closes the internal opening from inside the anal canal using stitches and staples.
Colostomy to allow healing in rare cases