Causes
Most anal fissures are caused by stretching of the anal mucous membrane beyond its capability.
Superficial or shallow anal fissures look much like a paper cut, and may be hard to detect upon visual inspection; they will generally self-heal within a couple of weeks. However, some anal fissures become chronic and deep and will not heal. The most common cause of non-healing is spasming of the internal anal sphincter muscle which results in impaired blood supply to the anal mucosa. The result is a non-healing ulcer, which may become infected by fecal bacteria. In adults, fissures may be caused by constipation, the passing of large, hard stools, or by prolonged diarrhea. In older adults, anal fissures may be caused by decreased blood flow to the area. When fissures are found laterally, tuberculosis, occult abscesses, leukemic infiltrates, carcinoma, acquired immunodeficiency syndrome (AIDS) or inflammatory bowel disease should be considered as causes. Some sexually transmitted infections can promote the breakdown of tissue resulting in a fissure. Examples of sexually transmitted infections that may affect the anorectal area are syphilis, herpes, chlamydia and human papilloma virus.
Other common causes of anal fissures include:
- Childbirth trauma in women
- Crohn's disease
- Plcerative colitis
- Poor toileting in young children.
- Anal trauma
Signs and symptoms
Severe pain during a bowel movement is the most common symptom of an anal fissure. In some cases, the pain may last for hours after your bowel movement. You may also observe blood on your stool or toilet paper. Upon visual inspection, you may be able to see the crack in your tissue or notice a skin tag near the injury. If you're experiencing these symptoms, your specialist at Progressive Surgical Care evaluates you to confirm if you have an anal fissure. During your examination, your specialist determines if your anal fissure is acute or chronic. Most fissures can be treated conservatively with medications, creams, and change in diet.
Diagnosis
External anal fissures on the anal verge can be diagnosed by visual inspection. Internal anal fissures in adults on anterior side, posterior side or within any part of the inner circumference of the anal sphincter muscle can be diagnosed with q proctoscope or by digital rectal examination with a finger inside the anal sphincter muscle. Narrow anal fissures might not be felt by finger during rectal examination due to the glove.
Treatment
Surgical procedures are generally reserved for people with anal fissure who have tried medical therapy for at least one to three months and have not healed. It is not the first option in treatment.
The main concern with surgery is the development of anal incontinence. Anal incontinence can include the inability to control gas, mild fecal soiling, or loss of solid stool. Some degree of incontinence can occur in up to 45 percent of patients in the immediate surgical recovery period. However, incontinence is rarely permanent and is usually mild. The risk should be discussed with one's surgeon.
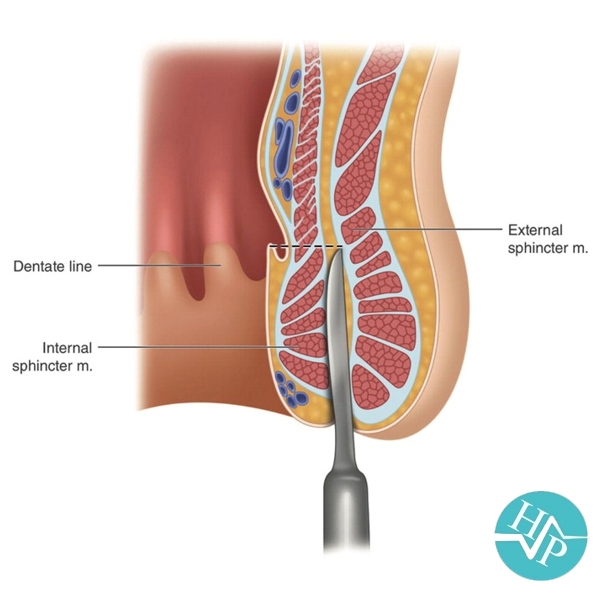
Surgical treatment, under general anaesthesia, was either anal stretch (Lord's operation) or lateral sphincterotomy where the internal anal sphincter muscle is incised. Both operations aim to decrease sphincter spasming and thereby restore normal blood supply to the anal mucosa. Surgical operations involve a general or regional anaesthesia. Anal stretch is also associated with anal incontinence in a small proportion of cases and thus sphincterotomy is the operation of choice.
Anal dilation, or stretching of the anal canal (Lord's operation), has fallen out of favour in recent years, primarily due to the unacceptably high incidence of fecal
incontinence.[29] In addition, anal stretching can increase the rate of flatus
incontinence. The incidence of incontinence is thought to be due to a lack of
standardization and that proper technique results in little chance that it will
occur.
In the early 1990s, however, a repeatable method of anal dilation proved to be very effective and showed a very low incidence of side effects.[32] Since then, at least one other controlled, randomized study has shown there to be little difference in healing rates and complications between controlled anal dilation and LIS,[33]
while another has again shown high success rates with anal dilation coupled with
low incidence of side effects.
Botox injection is also effective for treating Anal Fissure or Anal Pain. Most patients have at least some relief in their pain after treatment with Botox. In about one half (50%) of patients the pain goes away completely. It usually takes about 1 to 2 weeks to start feeling relief.
Lateral internal sphincterotomy (LIS) is the surgical procedure of choice for anal fissures due to its simplicity and its high success rate (~95%). In this procedure the internal anal sphincter is partially divided in order to reduce spasming and thus improve the blood supply to the perianal area. This improvement in the blood supply helps to heal the fissure, and the weakening of the sphincter is also believed to reduce the potential for recurrence. The procedure is generally performed as a day surgery after the patient is given general anesthesia. The pain from the sphincterotomy is usually mild and is often less than the pain of the fissure itself. Patients often return to normal activity within one week. LIS does, however, have a number of potential side effects including problems with incision site healing and incontinence to flatus and faeces (some surveys of surgical results suggest incontinence rates of up to 36%). Though lateral internal sphincterotomy (LIS) is considered safe on a short-term basis, there are concerns about its long-term safety. Pankaj Garg et al. published a systematic review and meta-analysis in which they analyzed the long-term continence disturbance two years after the LIS procedure. They found the incidence of long-term continence disturbance to be 14%, so caution and careful patient selection are needed before undergoing LIS.
Fissurectomy involves excision of the skin on and around the anal fissure and excision of the sentinel pile if one is present. The surgical wound can be left open. New skin tissue grows and it
heals.