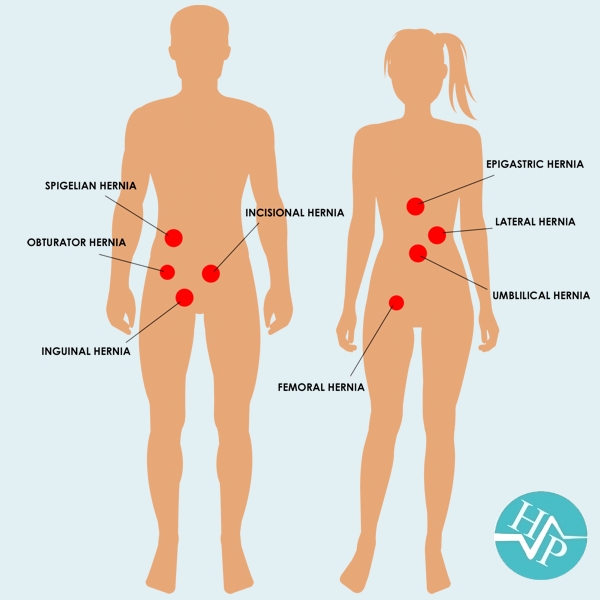
Types of hernias
Some of the most common types of hernias are explained below.
-
Inguinal hernias, in the inner groin area, occur when the
intestine protrudes through either of two passages in the lower abdominal
wall called inguinal canals. Researchers have estimated that about 27% of
men and 3% of women will develop an inguinal hernia at some point in their
lives.
-
Femoral hernias, in the upper thigh/outer groin area, occur in
deeper passages called femoral canals. They are much less common than
inguinal hernias and are far more likely to occur in women than in men. They
also present a higher risk of complications if they are not repaired.
-
Ventral hernias occur through an opening in the muscles of the
abdomen. There are three types of ventral hernias:
- Epigastric hernias occur
above the bellybutton.
- Spigelian hernia occurs through slit like defect in the anterior abdominal wall adjacent to the semilunar line
- Incisional hernias are
caused by a weakening of the abdominal muscle resulting from an incision
made during a previous abdominal surgery.
- Umbilical hernias, which
occur near the bellybutton, are most common in newborns, especially those
born prematurely. These hernias usually close on their own by the time the
child turns 4. Umbilical hernias can be more problematic when they occur in
adults.
-
Hiatal hernias occur when the upper part of the stomach bulges
into the chest through a small opening (the hiatus) in the diaphragm. The
hiatus allows the oesophagus, which carries food from the mouth to the
stomach, to pass through the diaphragm.
Causes
Furthermore, conditions that increase the pressure in the abdominal cavity may also cause hernias or worsen existing ones. Some examples would be: obesity, straining during a bowel movement or urination (constipation, enlarged prostate), chronic lung disease, and fluid in the abdominal cavity (ascites). Also, if muscles are weakened due to poor nutrition, smoking, or overexertion, hernias are more likely to occur. The physiological school of thought contends that in the case of an inguinal hernia, the above-mentioned symptoms are only an anatomical symptom of the underlying physiological cause. They contend that the risk of hernia is due to a physiological difference between patients who have hernia and those who do not, namely the presence of aponeurotic extensions from the transversus abdominis aponeurotic arch. Abdominal wall hernias may occur due to trauma. If this type of hernia is due to blunt trauma, it is an emergency condition and could be associated with various solid organ and hollow viscus injuries.
Signs and symptoms
For most people, hernias do not present with any symptoms other than the lump itself. However, if you experience a number of symptoms, including sudden, severe pain, vomiting, constipation, or wind, a tenderness in the area of the hernia, and being unable to push the hernia back in, this may mean that your hernia has become 'strangulated' and you should seek immediate medical treatment. If you suspect you have a hernia, your first port of call should be to your GP, who can assess you. He or she may decide that you need treatment, in which case you will be referred for a surgical consultation.
Diagnosis
A physical exam is usually all that's needed to diagnose an inguinal hernia. Our doctor will check for a bulge in the abdominal wall and groin. Because standing and coughing can make a hernia more prominent, you'll likely be asked to stand and cough or strain. If the diagnosis isn't readily apparent, we might order an imaging test, such as an abdominal ultrasound, CT scan or MRI.
Treatment
"Watchful waiting" is considered a potential alternative to surgery when a hernia is causing minimal or no symptoms. People who delay surgery, especially men with an inguinal hernia, should watch for symptoms and see a doctor regularly. About 70% of men with an inguinal hernia who delay surgery will develop new or worsening symptoms and will need surgery within five years. One risk of waiting too long is that a larger hernia is more difficult to repair.
Surgery is recommended for some types of hernias to
prevent complications such as obstruction of the bowel or strangulation of the
tissue, although umbilical hernias and hiatus hernias may be watched or treated
with medication. Most abdominal hernias can be surgically repaired, but surgery
has complications. The time needed for recovery after treatment is reduced if
hernias are operated on laparoscopically. However, open surgery can sometimes be
done without general anaesthesia. Uncomplicated hernias are principally repaired
by pushing back, or "reducing", the herniated tissue and then mending the
weakness in muscle tissue (an operation called herniorrhaphy). If complications
have occurred, the surgeon will check the viability of the herniated organ and
remove part of it if necessary. Muscle reinforcement techniques often involve
synthetic materials (a mesh prosthesis). The mesh is placed either over the
defect (anterior repair) or under the defect (posterior repair). At times,
staples are used to keep the mesh in place. These mesh repair methods are often
called "tension-free" repairs because, unlike some suture methods (e.g.,
Shouldice), muscles are not pulled together under tension. However, this widely
used terminology is misleading, as there are many tension-free suture methods
that do not use mesh (e.g., Desarda, Guarnieri, Lipton-Estrin, etc.).